ASSISTED REPRODUCTION
- Home
- Blastocyst Transfer
Blastocyst Transfer

The ultimate goal of in vitro fertilization (IVF) is a normal single intrauterine pregnancy. The IVF process involves stimulation of egg development through the use of injectable medications referred to as gonadotropins. After retrieval of the eggs and fertilization, embryos are produced which we hope are capable of continued normal development leading to a successful pregnancy.
We now know that under standard IVF culture conditions, only about 10 to 20% of fertilized eggs will progress to become a normal pregnancy. The challenge for our team is choosing the embryos most likely to result in a normal pregnancy. Accurate selection of these embryos enables the clinician to transfer fewer eggs, leading to fewer multiple pregnancies, and ultimately a higher pregnancy rate.
Over the past several years, in vitro culture conditions have improved, enabling us to culture embryos for up to six days after retrieval. Normally, by this time the embryos have reached a stage of development called the blastocyst. This extended culture time enables nature to help select those embryos with the highest capacity to produce a pregnancy.

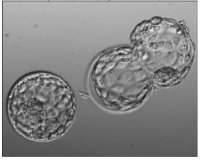
A blastocyst is an embryo that has developed for 5 days after fertilization and has divided into two different cell types. The surface cells, seen in the embryo on the right, are called the trophectoderm and will eventually become the placenta. The inner cell mass will become the fetus. A healthy blastocyst should hatch from its "shell" (zona pellucida) by the end of six days, and within 24 hours after hatching it should begin to implant within the lining of the uterus.
Recent studies have demonstrated that embryos that do not survive to the blastocyst stage have a very high incidence of abnormal chromosome numbers. Thus, allowing embryos to culture to the blastocyst stage significantly decreases the number of abnormal embryos.
The transfer of high-grade blastocysts has resulted in implantation rates between 40% and 50%. With the transfer of only two blastocyst embryos, pregnancy rates as high as 60% have resulted. These high implantation and pregnancy rates are due, in large part, to nature's selection of those embryos that have the highest chances of producing a pregnancy.
There are currently many unresolved issues regarding blastocyst transfer. Blastocyst transfer has a number of risks and accordingly is not appropriate for every couple. In a small percentage of patients, none of the embryos progresses to the blastocyst stage and gradually degenerates.This results in a complete loss of all embryos. There are many other unanswered questions. Will blastocyst transfer improve pregnancy rates for a few couples, for many couples, or for almost all couples undergoing IVF? How many blastocysts should we transfer for an acceptable pregnancy rate and a low multiple pregnancy rate? Which patients are the most appropriate for blastocyst transfer?
We at the pioneers in performing blastocyst culture and transfer. The decision to perform blastocyst culture and transfer is based on several factors including patient age, egg age in cases of donor egg, the number of eggs retrieved, previous IVF success, and perhaps most important, the embryo grade and cell count on day 3 of culture. We feel blastocyst culture and transfer has significant advantages for younger patients, egg recipients who receive eggs from younger donors, high responders (many eggs retrieved), or patients with previous IVF success. We encourage you to discuss the possibility of blastocyst transfer with your infertility physician.